Neurodegenerative diseases like Alzheimer’s and Parkinson’s are among the most challenging medical conditions of our time. Early detection and precise diagnosis are critical for effective treatment, yet these diseases often go unnoticed until significant progression has occurred. Enter Brainet and SimonMed, whose recent partnership is reshaping the future of neurodiagnostics through cutting-edge artificial intelligence (AI).
A Revolution in Healthcare
Brainet, a leader in neuroinformatics, has joined forces with SimonMed, one of the largest outpatient imaging providers in the United States. Together, they aim to leverage AI to improve the accuracy and efficiency of diagnosing neurodegenerative disorders. This collaboration represents a groundbreaking step forward, combining Brainet’s advanced AI algorithms with SimonMed’s extensive imaging infrastructure.
How AI is Changing Neurodiagnostics
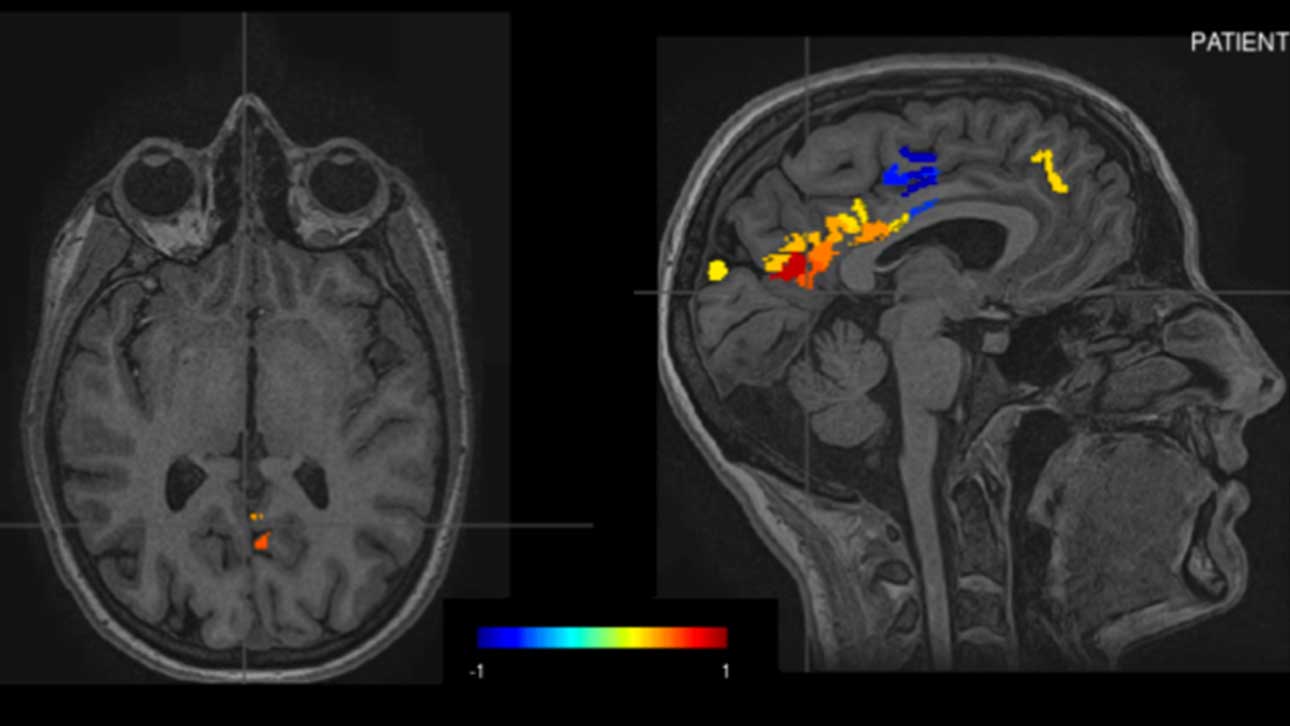
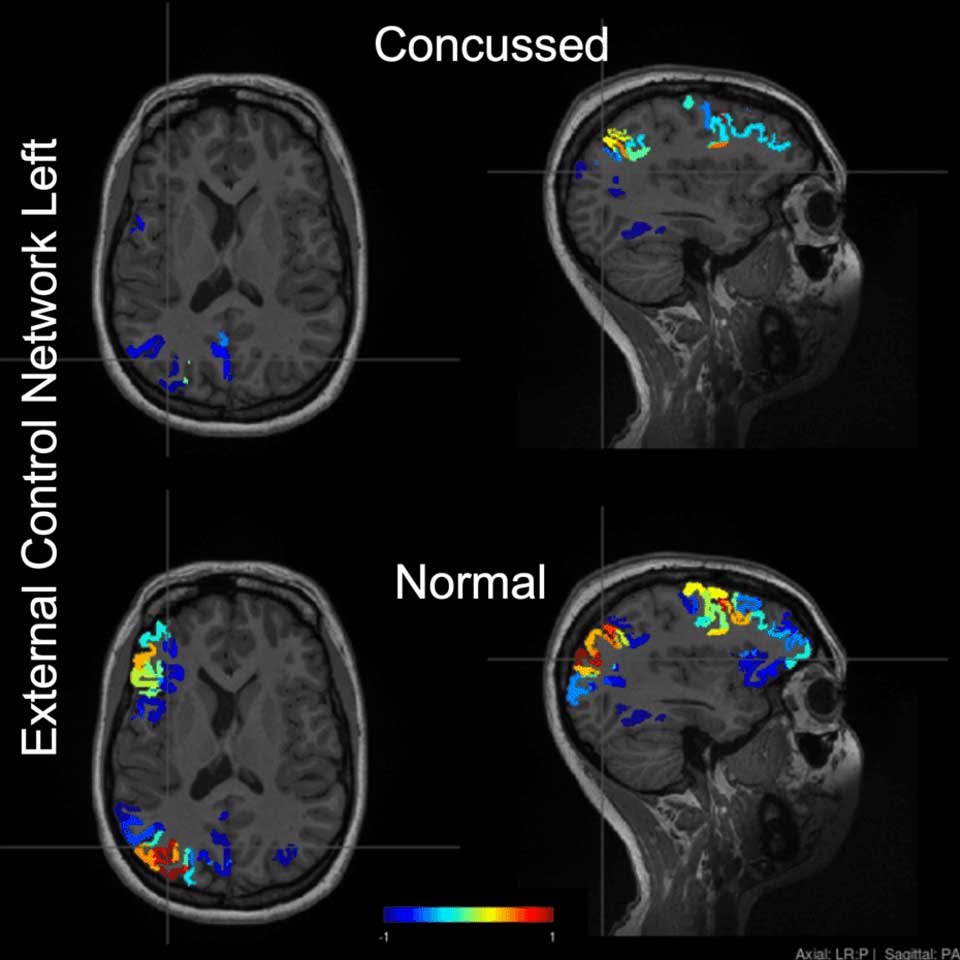
AI is revolutionizing how we analyze medical data, particularly in the realm of neuroimaging. Brainet’s AI tools are specifically designed to identify subtle changes in brain structure and activity, often undetectable by the human eye. These tools can:
- Enhance Diagnostic Accuracy: AI can identify patterns and anomalies that might be missed during manual analysis.
- Speed Up Diagnoses: Automated processes reduce the time required to analyze imaging data.
- Support Early Intervention: Detecting diseases at an earlier stage opens the door to timely and more effective treatments.
SimonMed’s network of imaging centers provides the ideal platform for deploying Brainet’s AI solutions, ensuring that patients across diverse regions can access advanced diagnostic tools.
Why This Matters
Traditionally, diagnosing neurodegenerative diseases has been a complex and subjective process. With AI, clinicians gain access to a standardized and data-driven approach, reducing the risk of misdiagnosis and improving patient outcomes.
For patients, this means:
- Earlier and more accurate detection of conditions like Alzheimer’s.
- Tailored treatment plans informed by precise data.
- Greater accessibility to cutting-edge diagnostic tools.
A Vision for the Future
This partnership is just the beginning. The integration of AI in neurodiagnostics opens the door to a range of possibilities, including:
- Personalized Medicine: Developing customized treatment plans based on detailed AI analysis.
- Enhanced Research Opportunities: Gaining deeper insights into the mechanisms of neurodegenerative diseases.
- Wider Accessibility: Making advanced diagnostics available to underserved populations.
Brainet and SimonMed’s collaboration sets a powerful example for how technology and healthcare providers can work together to address critical challenges in medicine.
Join the Movement
Are you a healthcare professional, researcher, or technology innovator? This groundbreaking initiative highlights the importance of collaboration in advancing medical science. Brainet and SimonMed invite you to contribute to this exciting frontier. Whether through partnerships, research, or technology development, there’s a role for everyone in shaping the future of neurodiagnostics.
Stay Updated!
The partnership between Brainet and SimonMed is more than a technological innovation; it’s a transformative step toward better health outcomes for millions of people. By combining the power of AI with a commitment to accessibility and precision, they are redefining what’s possible in neurodiagnostics.
Stay updated with this revolutionary collaboration and explore how you can be part of this journey. Together, we can create a future where early diagnosis and effective treatment of neurodegenerative diseases are the norm, not the exception.